COVID-19 Forecast for El Paso County – June 30
Plus, our resident microbiologist on ‘guilt-free’ testing and coronavirus hotspots
Good morning, and happy Tuesday. On this pre-pandemic date last year, 85 motorists raced their way up Pikes Peak in the annual Broadmoor Pikes Peak International Hill Climb. (This year, the race is scheduled for Aug. 30 — without spectators).
Today, our resident microbiologist Phoebe Lostroh returns to give her weekly COVID-19 forecast for El Paso County and to explain why “guilt-free” testing is an integral part of Colorado College’s plan for fall. Lostroh is a professor of molecular biology at Colorado College on scholarly leave who is serving as the program director in Genetic Mechanisms, Molecular and Cellular Biosciences at the National Science Foundation. She has a contract to write a “Pocket Guide” to SARS-Coronavirus-2.
➡️ICYMI: Yesterday, we explained Colorado College’s plan for the coming fall semester and the questions the college will need to answer next.
Phoebe’s Forecasts
NOTES: These forecasts represent her own opinion and not necessarily those of the National Science Foundation or Colorado College. She used the public El Paso County dashboard for all data.
⚖️ How her predictions last week fared: June 26 is the last day of Morbidity and Mortality Weekly Report week 26 in the national public health calendar. It is also during the 17th week since the first case was detected in El Paso County. Since March 13, 112 El Paso County residents have died of COVID-19. Last week, using the most recent trend, Lostroh forecasted 2,282 cumulative reported cases as of June 26 and in reality, there were 2,307 reported cases. Because the spread of an infectious disease through a susceptible population is exponential, this tiny difference in a short time frame can make a big difference in a matter of weeks if the increasing trend continues.
Predicted cumulative reported cases in El Paso County

Forecasted reported cases for June 30 to July 28

🗝️ Key points: Compared with last week, the most likely forecast is worse and is similar to the worst-case scenario for the next two weeks.
14-day incidence in El Paso County using reported cases

🗝️ Key points: Another way to try to predict how the number of newly-reported cases will change in the short term is to consider the 14-day incidence, which requires adding up all cases reported in 14 days and dividing by 7.15 (because there are 715,000 Springs residents). The horizontal dotted lines show the thresholds the Colorado Department of Public Health uses to make policy decisions. If people hadn’t complied with Stay-at-Home, we probably would have reached the “high” threshold about April 21. We entered the “high viral spread” zone several days ago, and I project that we will remain in this zone for the next four weeks, as indicated by the green “recent” forecasting curve above.
What do the different “Statuses of Viral Spread” mean?
The Colorado Department of Public Health defines them as follows:
Low:
25 or fewer new cases per 100,000 people in the 14-day rolling average in the context of stable or declining cases, excluding cases associated with outbreaks in residential facilities. Or, in counties with “high testing rates,” a two-week positivity rate of less than 5%.
AND:
Stable or declining average hospitalizations in the county’s referral hospitals.
Medium
50 or fewer new cases per 100,000 people in the 14-day rolling average in the context of stable or declining cases, excluding cases associated with outbreaks in residential facilities. Or, in counties with “high testing rates,” a two-week positivity rate of less than 10%.
AND:
Stable or declining average hospitalizations in the county’s referral hospitals.
High
50-100 new cases per 100,000 people in the 14-day rolling average in the context of stable or declining cases, excluding cases associated with outbreaks in residential facilities. Or, in counties with “high testing rates,” a two-week positivity rate of less than 15%.
AND:
Stable or declining average hospitalizations in the county’s referral hospitals.
Compare testing and viral spread
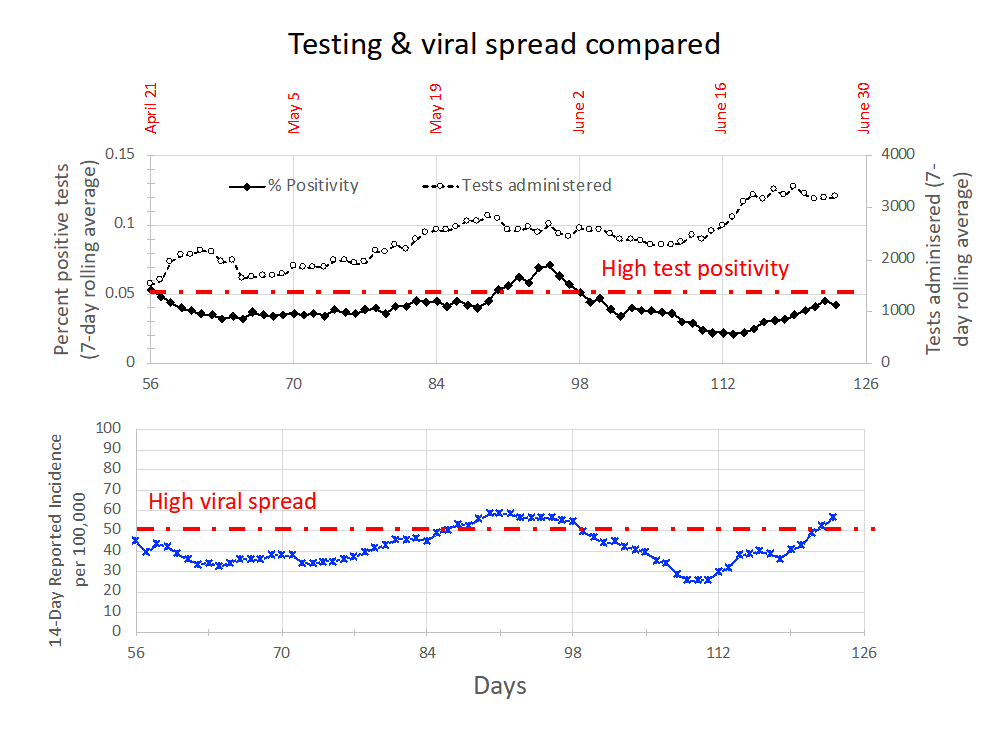
🗝️ Key points: The above graph documents the seven-day rolling average for nasal swabs for viral genomes in the upper respiratory tract, which are sometimes referred to as “PCR tests.” The top panel of this figure shows the percent positive tests with the black dots (left axis) and the tests administered with the white dots (right axis). From June 10-19, the number of total tests increases with almost exactly the same pattern as the percent positive tests decline. The percent positivity has increased steadily, getting close to the 5% “high positivity” mark. Thus, I believe our percent positivity of tests has been increasing steadily for about a week.
In combination with our entering the “high viral spread” threshold for the 14-day rolling incidence and the dramatically changed exponential curve fit for the last seven days, I believe that we are heading into a period of higher COVID-19 caseloads.
Q-and-A with Lostroh: Our resident microbiologist reacts to CC’s plan for fall
This interview has been edited for length and clarity.
CC COVID-19 Reporting Project: As a microbiologist, what are your initial reactions to CC’s recently announced plan?
Lostroh: In terms of handling the physical spaces and thinking about how many people to have on campus at a time, how to handle a living experience, how to let everyone who can work from home, I think all those plans are as good as they possibly can be. But I’m concerned about the fundamental underlying question of whether it’s a good idea for people from all over the country right now to come together and what the plan is for if the situation in Colorado Springs itself changes for the worse.
CCRP: From your perspective, what could CC do to make campus as safe as possible?
Lostroh: What I would really like to see is a way to have absolutely no questions asked with testing. Anybody who wants to can get a test for any reason without having to explain at all. So I think that would help keep everybody safe, and I think it needs to be everybody — not just students, not just staff, not just faculty — anybody who shows up and says, “You know what? I think I need a test.” Guilt-free testing is really, really important. I listened to [White House Coronavirus Task Force coordinator] Deborah Birx give a seminar to the American Society for Microbiology last week. She told us that one of the most dangerous things anyone can do right now is to gather in large groups with people who are not from your local neighborhood. And we want people from all over the country and all over the world to be part of our Colorado College experience. That means that we are going to bring together hundreds of people from all over the country, in a short period of time. And to me, that sounds a lot like exactly what Dr. Birx would like for us not to do. So it concerns me that no matter what our plans are for detecting and tracing cases, just bringing people from all over together is going to be a certain amount of risk. And my experience with CC is that we have a lot of students who come from Texas, Arizona, California, Nevada, Utah, and Wyoming. We draw on a group of people who are from the states that are having outbreaks right now. Maybe those outbreaks will be resolved by the time August comes around. I think that could be true. It depends on how fast the curve goes down.
The other thing I would like us to be clearer on with everyone is what happens if the local situation in Colorado Springs changes. Are there any thresholds for hospital capacity or cases in our zip code that would make the college change its mind about the safety of people being on campus? The problem with exponential growth is that when you notice it’s getting bad, you should have done something about it a week or two ago.
CCRP: What new developments in coronavirus research are you keeping an eye on?
Lostroh: There are these really interesting experiments where cell biologists have figured out how to grow cells in communities in the lab instead of just separately. They can make what they call “organoids,” which don’t look like a little kidney or a little liver, but they have cells and communities that kind of behave more like an intact organ would. They’ve been doing experiments with these organoids to try to figure out if the virus infects exclusively lung cells, or if it’s infecting more, different kinds of cells in the body. And it turns out that yes, the virus is infecting way more cells in the body than anybody would have predicted based on what we knew about it at the beginning of the outbreak.
About the CC COVID-19 Reporting Project
The CC COVID-19 Reporting Project is a student-faculty collaboration by Colorado College student journalists Miriam Brown and Arielle Gordon, Visiting Assistant Professor of Journalism Corey Hutchins, Assistant Professor of English Najnin Islam, and Journalism Institute Director Steven Hayward. Work by Phoebe Lostroh, Associate Professor of Molecular Biology at CC and National Science Foundation Program Director in Genetic Mechanisms, Molecular and Cellular Biosciences, will appear from time to time, as will infographics by Colorado College students Rana Abdu, Aleesa Chua, Sara Dixon, Jia Mei, and Lindsey Smith.
The project seeks to provide frequent updates about CC and other higher education institutions during the pandemic by providing original reporting, analysis, interviews with campus leaders, and context about what state and national headlines mean for the CC community.
📬 Enter your email address to subscribe and get the newsletter in your inbox each time it comes out. You can reach us with questions, feedback, or news tips by emailing ccreportingproject@gmail.com.


