COVID-19 Forecast for El Paso County – June 15
Plus, Phoebe Lostroh talks asymptomatic transmission and the WHO
Good morning, and happy Monday!
Today, Phoebe Lostroh returns to give her weekly COVID-19 forecast for El Paso County. She’ll also talk about the difference between “asymptomatic” and “presymptomatic” transmission. Lostroh is a professor of molecular biology at Colorado College on scholarly leave who is serving as the program director in Genetic Mechanisms, Molecular and Cellular Biosciences at the National Science Foundation.
➡️ICYMI: On Friday, we explained a new variance allowing family to attend El Paso County high school graduations, provided updates on Colorado College’s voluntary furlough program, and rounded up some recent student journalism.
Phoebe’s Forecasts
NOTES: These forecasts represent her own opinion and not necessarily those of the National Science Foundation or Colorado College. She used the public El Paso County dashboard for all data.
⚖️How her predictions last week shaped up: Using the most recent trend (“best guess”), I forecasted 134 new cases reported as of June 11 — but there were only 62. My estimate for newly-reported cases was too high by a large margin. June 11 was the beginning of the 15th week since the first case was detected in El Paso County; 102 county residents have died of COVID-19 since March 5. Last week, using the most recent trend (“best guess”), I forecasted 2,000 cumulative reported cases as of June 11, and in reality, there were 1,928 reported cases. My estimate was thus too high for reported cases.
My number of forecasted reported cases in the next weeks has decreased further because the total number of new reported cases has declined for two weeks in a row. New reported cases are only 60% of what they were two weeks ago. If the current trajectory of cases continues, we have sufficient hospital capacity for the next six weeks and will not exceed the number of cases that would lead the state to retract the variance allowing restaurants to remain open.
🤔This decline in new cases reported since May 28 remains puzzling. Reported cases are declining in Colorado when averaged across all counties, so El Paso County is not anomalous in that regard. When considering my analysis, keep in mind that I have been analyzing reported cases, not actual cases. It is normal in any outbreak for reported cases to be lower than actual cases.
Predicted cumulative reported cases in El Paso County
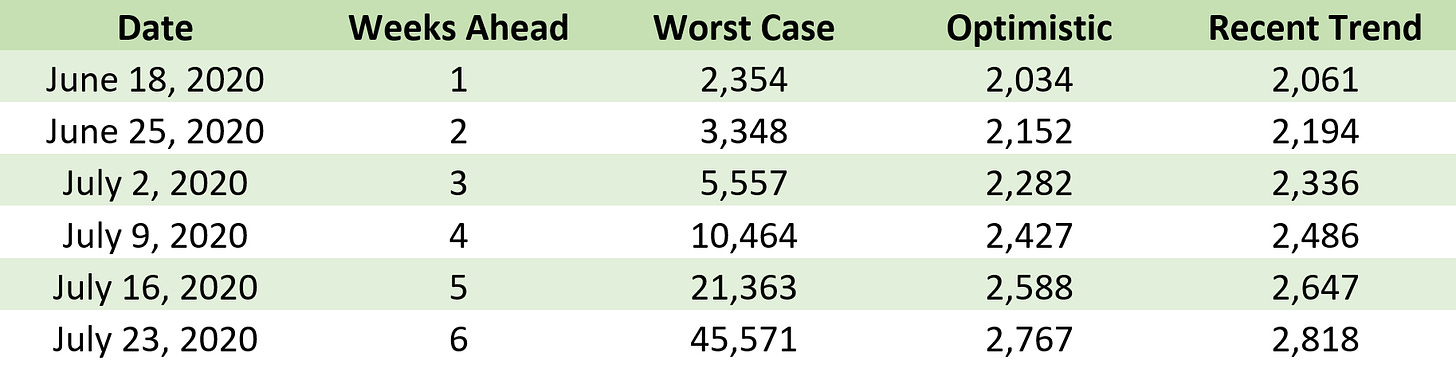
Predicted new COVID-19 reported cases in El Paso County

COVID-19 comparisons with Colorado’s geographical neighbors
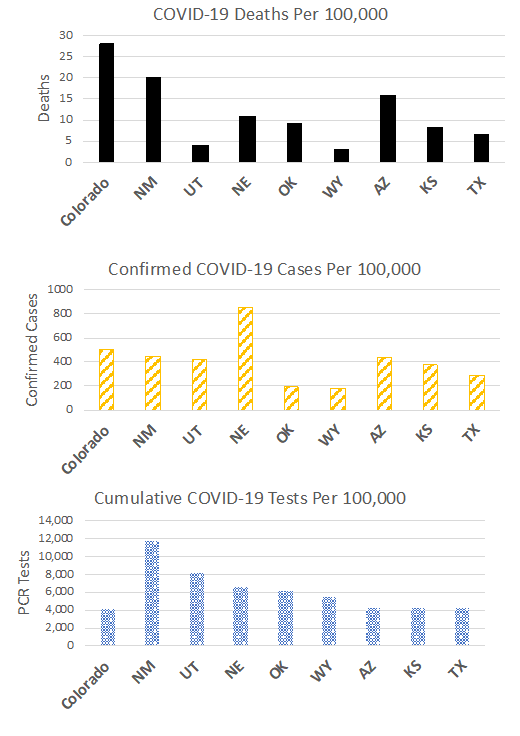
🗝️Key points: As of today, our neighbors with increasing cases include New Mexico, Arizona, Utah, Wyoming, Oklahoma, and Texas, while cases are declining in Kansas and Nebraska. Compared with our neighbors, we have had higher COVID-19 death rates (normalized by state population) than all of them. We have had about half as many confirmed cases per 100,000 people as Nebraska but more confirmed cases per 100,000 than all of the rest of our geographical neighbors. We have performed fewer “PCR tests” per 100,000 people than all of our geographical neighbors. Considering all 50 states, the District of Columbia, and Puerto Rico, the state of Colorado has the fifth lowest rate of testing (normalized by population).
Testing and positivity rate in El Paso County each week
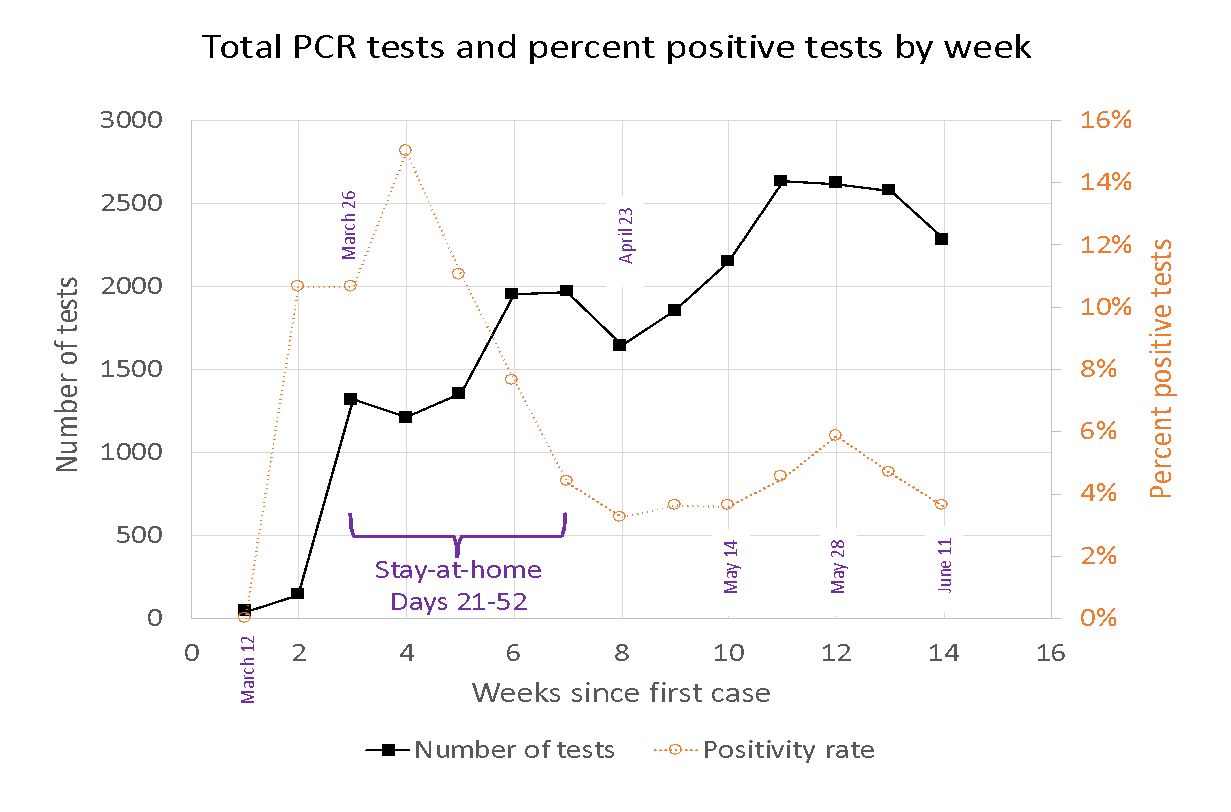
🗝️Key points: El Paso County’s testing rate was lower this past week than it was earlier in the outbreak. The maximum number of such tests in El Paso County in any week since the outbreak began was 2,630 tests, performed during the 10th week of the outbreak. During the most recent week, 2,270 tests were performed, which is a 13% drop in testing compared to the maximum week. A decline in testing rates is not desirable, as it could indicate that people with symptoms are not getting the tests. The percent positive rate is still hovering around 4%, however, which is good, because it indicates that testing is sufficient to catch positive cases in the communities getting tested.
Cumulative reported cases for El Paso County
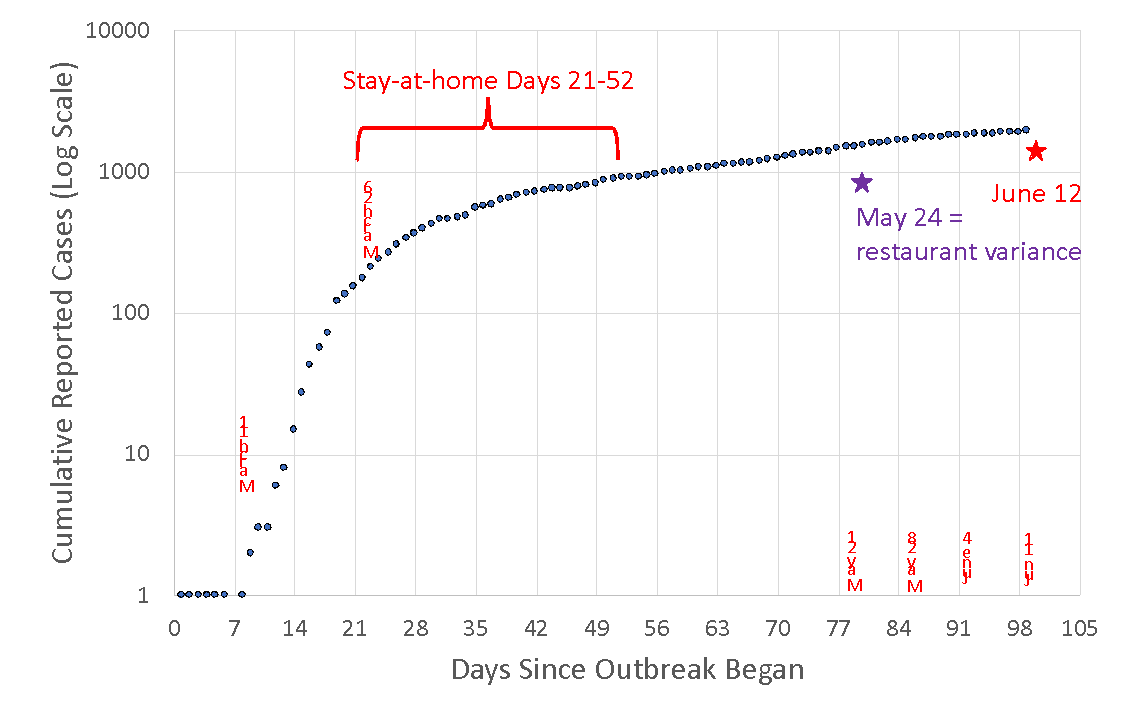
🗝️Key points: Data from June 5 to June 12 have the most uncertainty because most changes to case data occur within one week of reporting. Many western states are experiencing a surge in cases attributed to Memorial Day Weekend gatherings, but we are not seeing such an increase in Colorado or in El Paso County.
Define portions of curve used for forecasting: Forecasting stages 1, 2, and 3
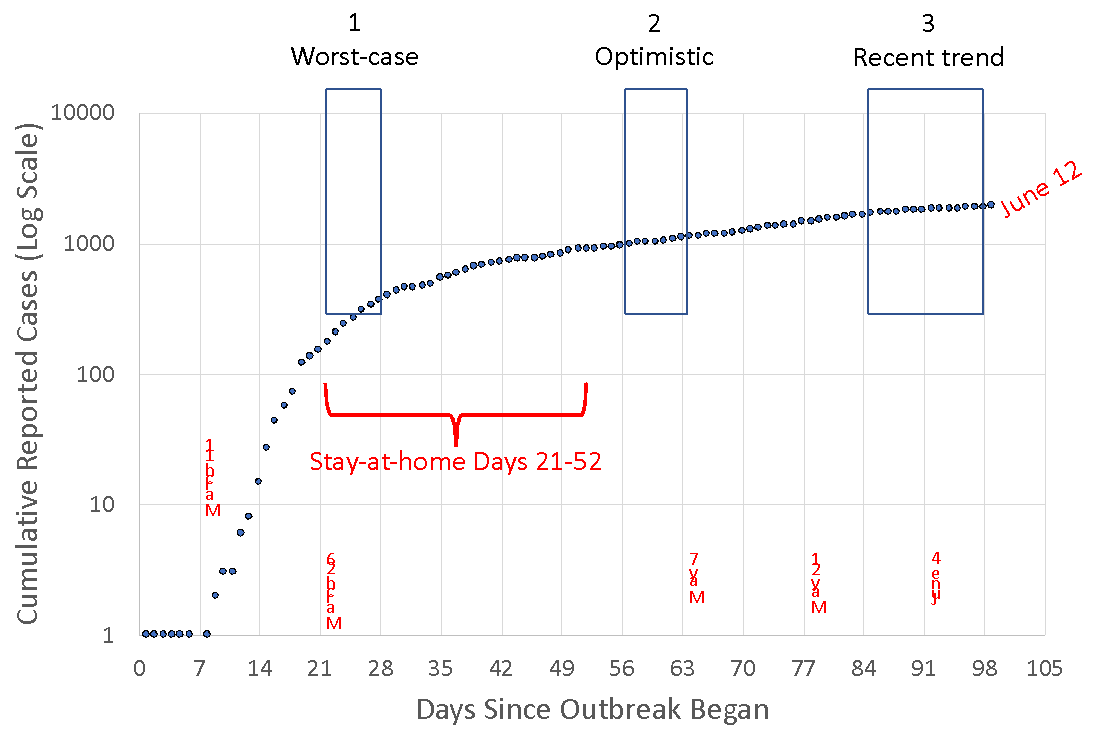
Forecast for the next four weeks of cumulative cases based on stages 1, 2, and 3
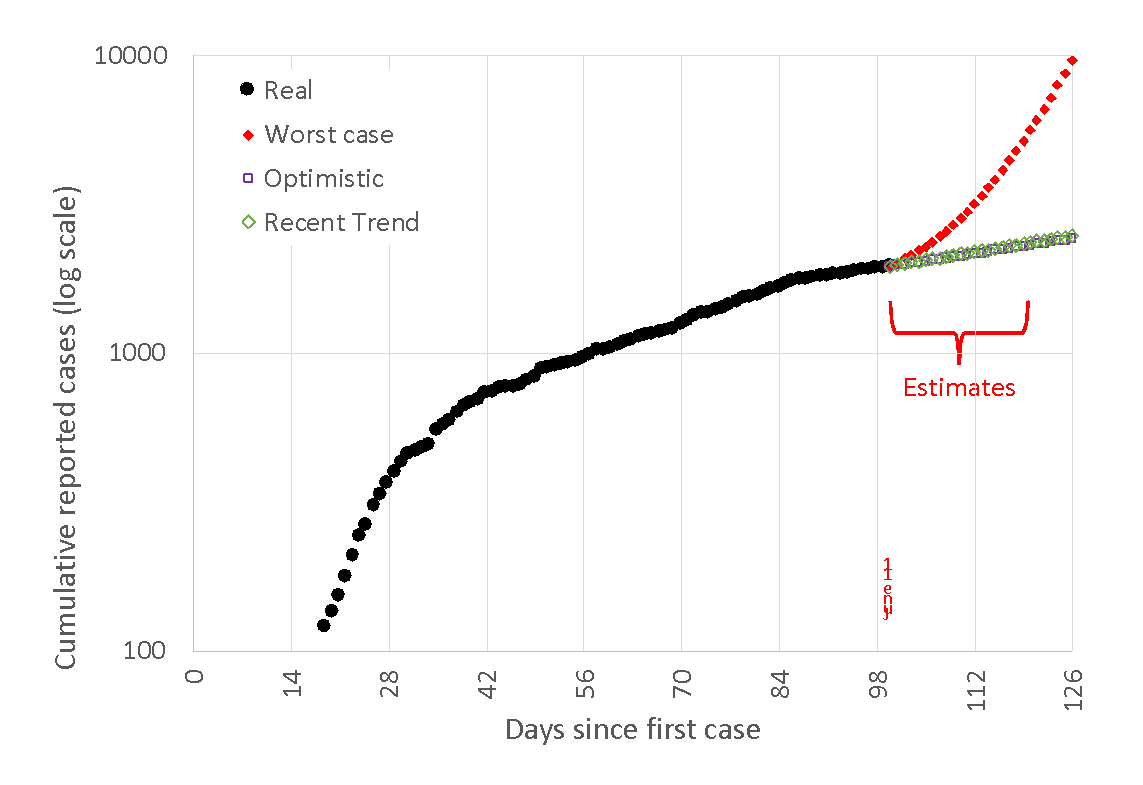
🗝️Key points: We are very far from the worst-case scenario, which would quickly overwhelm our local hospitals. Compared with last week, the best-guess scenario based on the most recent trend has gotten closer to the most optimistic prediction.
‘Asymptomatic’ vs. ‘presymptomatic’: Q-and-A with Lostroh, our resident microbiologist
This interview has been edited for length and clarity.
CC COVID-19 Reporting Project: OK, so first: what is the difference between ‘asymptomatic’ and ‘presymptomatic’ transmission?
Lostroh: That distinction has caused a lot of confusion. In everyday language, ‘asymptomatic’ means someone who doesn’t have symptoms or signs of the disease, but in medical science, it means someone who never shows signs of an infectious disease, whereas ‘presymptomatic’ means that someone who will eventually show signs and symptoms doesn’t have them yet. Doctors distinguish between ‘asymptomatic’ and ‘presymptomatic,’ whereas I think the general public thinks that asymptomatic includes both of those ideas.
CCRP: And why now? Why are we just now talking about the differences between those two terms? How is this connected to wearing masks?
Lostroh: In the United States, there was a severe mask shortage. There still is a shortage of N-95 masks in some healthcare settings, but there was a shortage of all medical masks. The Centers for Disease Control, knowing American culture and that there was a shortage of masks for healthcare personnel, decided to recommend against wearing face coverings. I think that was a big mistake, and I think there are some who are acknowledging that mistake now. The reason it was a mistake is that most of the people who have COVID-19 are not symptomatic yet spreading it for one to three days before they develop symptoms. The way you prevent spreading the virus to other people is by wearing a mask, even when you don’t have symptoms, because there’s no way to know if you’re going to develop symptoms or not. I think it is coming up as a concept right now because the idea of wearing face coverings is so important. It’s somewhat important for keeping yourself safe, but it’s very important for keeping other people safe because you may be presymptomatic, on your way to developing COVID-19 symptoms and you don’t know it yet, but you’re still spreading the virus into the air as you breathe.
CCRP: We’ve seen some headlines surrounding the World Health Organization and asymptomatic spread; could you tell us what exactly happened, and why they had to clarify a statement about asymptomatic transmission?
Lostroh: The WHO statement failed to take into account that for the public, asymptomatic and presymptomatic are synonymous. The official was really talking about asymptomatic infections, which would be people who had the infection and are spreading it, but literally never develop any signs or symptoms of the disease. As far as we know that is very rare, but there are strong examples in the peer-reviewed literature measuring transmission by people who eventually develop symptoms, or who were asymptomatic for some number of days before they develop those symptoms. Now the average number of days that someone is presymptomatic is probably around three, but it can be as few as one, or as many as seven, or maybe even longer. That’s another reason why it’s difficult to measure presymptomatic versus asymptomatic in the medical sense. If someone is presymptomatic for seven days, but you only follow them for three, you might misclassify them as asymptomatic and say they never got the infection. So it’s a difficult distinction to measure. There is peer-reviewed literature that 41% of infections in some cases are being spread by people who have no symptoms. That’s a huge number.
CCRP: We’re seeing a lot of debate right now about whether we’re entering a ‘second wave’ of the coronavirus or never quite finished the ‘first wave.’ Where do you stand on that?
Lostroh: This idea of ‘waves’ of infection comes directly from studies of the 1918-19 influenza pandemic. There was a period of like four months where the influenza was spreading, and then there was a period of three or four months where it went away. No one knew why and everybody thought they were safe, and then it came back for another three or four months and that peak was even higher in terms of incidents all over the world. So those were the ‘waves’ of the influenza pandemic. By analogy, people have been thinking maybe COVID-19 will also occur in waves. People still think that might happen. On a national level, it looks like the United States as a whole is still in the middle of an upswing overall. So is that the ‘first wave’? First implies there will be a second. We don’t know if there will be a second. If the virus is seasonal, it might just keep increasing. So there are lots of aspects of the wave theory that are unproven and difficult to predict at this time.
I think people are getting frustrated because the scientific messages that are coming out are not always clear, and sometimes contradict one another. I want people to get the message that, unfortunately, we are in the middle of a pandemic and learning new things about it as we go. I really rely on the free newsletter from the journal Nature. I rely on the free COVID-19 related news articles coming out of the American Association for the Advancement of Science, which publishes Science Magazine. Another source of high quality journalism on COVID-19 is STAT News. The other thing all those sources have in common is that they always link to the primary literature, so you know exactly the source of the information that’s been condensed.
About the CC COVID-19 Reporting Project
The CC COVID-19 Reporting Project is a student-faculty collaboration by Colorado College student journalists Miriam Brown and Arielle Gordon, Visiting Assistant Professor of Journalism Corey Hutchins, Assistant Professor of English Najnin Islam, and Journalism Institute Director Steven Hayward. Work by Phoebe Lostroh, Associate Professor of Molecular Biology at CC and National Science Foundation Program Director in Genetic Mechanisms, Molecular and Cellular Biosciences, will appear from time to time, as will infographics by Colorado College students Rana Abdu, Aleesa Chua, Sara Dixon, Jia Mei, and Lindsey Smith.
The project seeks to provide frequent updates about CC and other higher education institutions during the pandemic by providing original reporting, analysis, interviews with campus leaders, and context about what state and national headlines mean for the CC community.
📬 Enter your email address to subscribe and get the newsletter in your inbox each time it comes out. You can reach us with questions, feedback, or news tips by emailing ccreportingproject@gmail.com.