Good morning, and happy Tuesday!
Fasten that mask a little tighter, because today Phoebe Lostroh is returning to talk about a hypothesis that SARS Coronavirus-2 could be spread not only by droplets, but also by ... “aerosols.”
🌬️In recent weeks, some headlines have bubbled up about this potential. “We cannot keep ignoring the possibility of airborne transmission. Here’s how to address it,” was one in The Washington Post written by the director of Harvard’s Healthy Buildings program. Another WaPo headline read “Experiment shows human speech generates droplets that linger in the air for more than 8 minutes.” Meanwhile, “Both experimental and hospital studies have shown evidence of aerosol transmission of SARS-CoV-2,” reported the influential Lancet Medical Journal last week. The Centers for Disease Control, however, states the virus spreads primarily through “respiratory droplets produced when an infected person coughs, sneezes, or talks.”
Lostroh, a professor of molecular biology at Colorado College on scholarly leave who is serving as the program director in Genetic Mechanisms, Molecular and Cellular Biosciences at the National Science Foundation, is one of the microbiologists warning about the possibility of aerosol spread. Today we talk to her about why.
But first...
Phoebe’s Forecasts
NOTES: These forecasts represent her own opinion and not necessarily those of the National Science Foundation or Colorado College. She used the public El Paso County dashboard for all data.
How her predictions last week shaped up: The number of cases in the past week is lower than I predicted using my “best guess” strategy, which was 260 new cases between May 29-June 4. The “best guess” prediction was based on people behaving as we have been more recently, with some resuming activities and some choosing not to wear face coverings. Instead, there were only 130 new cases reported to El Paso County during that week. This number is very close to my “optimistic” prediction, which estimated 119 new cases in the same time interval. The “optimistic” prediction was based on people behaving as we did during the strictest Stay-at-Home order, and I know that El Paso County residents are no longer socially distancing to such an extreme degree. So, this contradiction between my prediction and the outcome surprised me.
Predicted cumulative cases

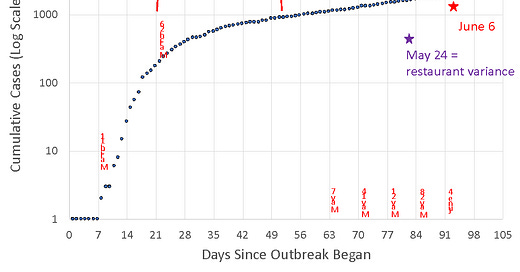
Cumulative COVID-19 cases, El Paso County, June 6

The plot shows that the outbreak has proceeded differently at different times. Between days 1-18, there was an explosive exponential increase. Then we see the curve flatten out from days 19-35, most likely as a consequence of actions taken prior to March 12. Notably, the Bridge Club that was the site of the first outbreak closed on March 12; on or around March 12, contact tracing began. Between days 35-63 or so, we see a pretty slow rise, most likely as a consequence of the Stay-at-Home orders and contact tracing followed by self-isolation as necessary. After day 63, we start to see the curve increasing a bit faster, especially as we leave the Stay-at-Home orders. Data from May 29-June 6 have the most uncertainty because most changes to case data occur within one week of reporting. Restaurants in Colorado Springs were allowed to open with limited capacity and some precautions starting on May 24.
Forecasting stages 1, 2, and 3

Stage 1 covers the last eight days of exponential increase before contact-tracing the earliest cases and the stay-at-home orders start to have an effect. Stage 2 captures the very end of Stay-at-Home and the first few days after we went to “Safer-at-Home,” and it is the flattest part of the curve of cumulative cases. Stage 3 is Lostroh’s best guess because it captures 14 data points while omitting today’s value, which will likely change because of a lag in reporting.
Lostroh Q&A: ‘A controversial hypothesis’
The following interview has been edited for length and clarity.
CC COVID-19 Reporting Project: Why aerosols, why now?
Phoebe Lostroh: I think that SARS Coronavirus-2 is being spread by aerosol, which was a controversial hypothesis several months ago. The spread is much harder to contain by aerosols than by droplets — but before I get into that it might be helpful to first distinguish between what’s a droplet and what’s an aerosol because those words sound like regular words, but they mean something very particular in medicine.
CCRP: OK — so what’s the difference between aerosols and droplets?
Lostroh: A droplet is a wet particle that is five microns or larger, which means about five to 10 times larger than a bacterium. Because droplets are that large, they are subject to gravity. When we exhale them, they fall to the ground. This business about saying you need to stay six feet away from someone is based on studies from the 1930s that show that droplets fall to the ground within about six feet from where someone is speaking.
CCRP: How different are aerosols?
Lostroh: An aerosol is much, much smaller. It’s still a respiratory particle. It’s still wet, but it can remain suspended in the air over much longer distances. And very importantly for infectious disease transmission, a tiny aerosol — which is about the same size as a bacteria or a few bacteria — can be inhaled deeply all the way down into the alveoli of the lungs, the little pouches where the air exchange actually happens. It’s in those specific little pouches, the alveoli, where the cells that are susceptible to SARS Coronavirus-2 actually are. So when the aerosol gets inhaled just through normal breathing into the lungs, it improves the opportunity of the virus to encounter the specific cells in our bodies that the virus can bind to and get inside.
CCRP: To put the range of aerosol transmission into context, the distance aerosols can travel is similar to the distance away that one can smell a barbecue grill or cigarette?
Lostroh: That’s right — if you can smell cigarette smoke or a barbecue, then that’s how far an aerosol could travel through the air and possibly be inhaled and infect someone. The precautions needed to protect yourself from an aerosol in a healthcare setting involve those N-95 masks that healthcare professionals are using. When it’s an aerosol you’re dealing with, it’s also a good idea to have eye protection if you are in an enclosed space with infectious aerosols. There was just a study out this week that shows that healthcare professionals who were using N-95 masks and goggles are better protected than healthcare professionals who are not wearing one or both of those.
CCRP: In terms of masks, would a bandana be effective?
Lostroh: A bandana would be able to help if it fit tightly against your face, but any homemade face protection device needs to fit tightly against the face to prevent aerosols from being inhaled because it’s around the edges of the mask, where the mask doesn't quite fit flush against your cheeks, that aerosols can come in. I saw a suggestion on NPR about using cut nylon stockings to tie that on top of your homemade face covering so that it stays tighter against your face.
CCRP: What are the implications in terms of colleges reopening in the fall?
Lostroh: I would really like to see us consider improving ventilation systems for indoor work in a school setting. There’s a professional society of HVAC engineers that recommends the HVAC system have three air exchanges per hour in order to reduce the likelihood of transmission. In terms of reopening, I would feel a lot more comfortable knowing that people are going to schools, classrooms and workplaces if those workplaces had been inspected and the HVAC systems had been modified if necessary to make sure that there are enough air exchanges per hour. This is a big implication for reopening. Another big implication for reopening is that the precaution of keeping six feet apart from one another is really based on droplet transmission. I think we need to wait and see what the advice is going to be from the CDC and other places about reducing aerosol transmission and not just droplet transmission. I know that mask wearing is going to be a part of the precautions we need to take for sure — wearing face coverings will absolutely help prevent anyone who is infected and doesn’t know it from spreading those aerosols to other people, as well as spreading droplets. SARS Coronavirus-2 is probably transmitted both with droplets and aerosol — but maybe six feet apart isn’t really enough. Or maybe we need to have more plexiglass separators in certain kinds of school or work settings. These kinds of things will have to be considered in more detail in light of transmission through smaller aerosols that can remain suspended in the air for longer periods of time, especially where there’s inadequate ventilation.
CCRP: So does that mean that the virus is “airborne”?
Lostroh: That term gets used casually in the media to refer to viruses that can be transmitted either by droplets or by aerosols. My experience in the professional literature is that scientists try to avoid using the word “airborne” and instead distinguish between droplet and aerosol transmission. That’s because it makes a big difference for healthcare workers in particular. For example, when a healthcare worker examines a person who has active tuberculosis, the doctor or nurse can actually contract tuberculosis from the patient just by being in the same room with them — because tuberculosis is transmitted by aerosol. That’s often not the case for other kinds of respiratory infections. This makes a big difference in a healthcare setting. Rather than the term “airborne,” I think we should stick with talking about droplet or aerosol transmission.
CCRP: What makes you so sure about an aerosol threat when the CDC isn’t really warning about it spreading this way?
Lostroh: Research moves faster than the Centers For Disease Control. I believe the biomedical research scientists who are releasing these results, and they want people to know about them.
CCRP: The protests across the country are on a lot of our minds right now, and many of us are taking part in them, or have family who are. Do you have any guidance or advice for the protesters, and how to stay safe?
Lostroh: My guidance is to stay as safe as you can while you are protesting, but also keep your family safe. Once you come home, self-quarantine and track your symptoms for two weeks. Make sure you’re not bringing home anything you could have caught at a protest to people who might be more vulnerable to infection. I really support the protesters, think it’s important and great that they’re out there, but this is a situation where somebody could bring the infection home to a grandparent or someone, and that it’s important to act responsibly in terms of the people who you live with. The point of the protest is to save lives, so please also protect the lives of the people that you're living with.
About the CC COVID-19 Reporting Project
➡️ICYMI: Yesterday, we rounded up news from across Colorado about an executive order allowing businesses to refuse service to customers without face coverings, what charter and public schools are discussing for the fall, and an update on antibody testing results.
The CC COVID-19 Reporting Project is a student-faculty collaboration by Colorado College student journalists Miriam Brown and Arielle Gordon, Visiting Assistant Professor of Journalism Corey Hutchins, Assistant Professor of English Najnin Islam, and Journalism Institute Director Steven Hayward. Work by Phoebe Lostroh, Associate Professor of Molecular Biology at CC and National Science Foundation Program Director in Genetic Mechanisms, Molecular and Cellular Biosciences, will appear from time to time.
The project seeks to provide frequent updates about CC and other higher education institutions during the pandemic by providing original reporting, analysis, interviews with campus leaders, and context about what state and national headlines mean for the CC community.
📬 Enter your email address to subscribe and get the newsletter in your inbox each time it comes out. You can reach us with questions, feedback, or news tips by emailing ccreportingproject@gmail.com.